Experiencing a miscarriage is one of the most physically and emotionally challenging events a person can go through. The grief is profound, often accompanied by a sense of emptiness that is hard to articulate. While you are navigating the emotional landscape of loss, your body is also undergoing significant physical changes.
After a miscarriage, your body must transition from a state of pregnancy back to its pre-pregnancy baseline. This involves a rapid drop in pregnancy hormones like human chorionic gonadotropin (hCG), estrogen, and progesterone. While this process is natural, these sudden shifts in postpartum hormones can sometimes lead to a lingering hormone imbalance.
This guide is designed to help you understand this often unspoken aspect of recovery. We will explore the common signs of hormone imbalance after a miscarriage, how healthcare providers diagnose it, and the paths available to help you find balance again. Please remember that what you are feeling—both physically and emotionally—is valid, and support is available.
Common Signs of Hormone Imbalance
When your hormones fluctuate wildly, it can feel as though your body is no longer your own. Identifying the symptoms is the first step toward understanding what is happening. While every individual’s experience is unique, several common signs indicate your hormones may be struggling to re-regulate.
Irregular Menstrual Cycles
One of the most prominent indicators of a hormone imbalance is a change in your menstrual cycle. After a miscarriage, it typically takes four to six weeks for your period to return, though this timeline can vary based on how far along the pregnancy was.
An “irregular” cycle might manifest as:
- Unusually long or short cycles: A cycle that deviates significantly from your typical 28-day rhythm.
- Heavy bleeding: Flow that is much heavier than what is normal for you.
- Spotting: Bleeding between periods or prolonged spotting before a full flow begins.
These irregularities often stem from the body’s attempt to restart ovulation and balance estrogen and progesterone levels. If these issues persist for several months, it is a strong signal that your hormones need support.
Persistent Mood Swings, Anxiety, or Depression
Grief is a natural and necessary part of healing from pregnancy loss. However, it is helpful to differentiate between situational grief and mood disturbances exacerbated by chemical imbalances.
A rapid drop in estrogen and progesterone—hormones that heavily influence brain chemistry—can lead to “baby blues” or postpartum depression, even after a miscarriage. You might experience irritability that feels uncontrollable, anxiety that keeps you on edge, or a depth of sadness that feels disproportionate to daily triggers. If these feelings persist or worsen over time, a hormone imbalance could be a contributing factor.
Chronic Fatigue and Sleep Disturbances
Are you feeling a level of exhaustion that sleep doesn’t seem to fix? This profound fatigue is common when hormones are out of sync. Progesterone has natural sleep-promoting/sedative properties. When progesterone levels plummet after a miscarriage, insomnia or restless sleep often follows.
Furthermore, the physical stress of the miscarriage combined with the emotional toll creates a perfect storm for adrenal fatigue, leaving you feeling drained and lethargic throughout the day.
Changes in Weight or Appetite
You may notice unexplained weight gain, particularly around the midsection, or sudden weight loss. These changes are often linked to cortisol, the body’s primary stress hormone. High stress levels can disrupt metabolism and increase cravings for sugar and carbohydrates.
Additionally, thyroid function can be temporarily impacted by the hormonal shifts of pregnancy and loss. If the thyroid slows down (hypothyroidism), weight gain becomes much easier, regardless of your diet or activity level.
Physical Symptoms: Acne, Hair Loss, and Libido
Your skin and hair are often mirrors of your internal health. A sudden onset of acne—specifically along the jawline—is a classic sign of hormonal fluctuation. You might also experience hair shedding or thinning (telogen effluvium) caused by the shock to the system.
A decreased libido is another common physical symptom. Between the emotional trauma of loss and low estrogen levels, a lack of desire for intimacy is a normal physiological response, yet it serves as another marker of hormonal disruption.
How is a Hormone Imbalance Diagnosed?
If you recognize these symptoms in yourself, please do not attempt to self-diagnose or “tough it out.” Consulting a medical professional is crucial for ensuring there are no underlying complications from the miscarriage (such as retained tissue) and for getting the right support.
The Medical Consultation
During your visit, your doctor will likely begin by discussing your medical history and the details of your miscarriage. They will ask about your symptoms—how long they have lasted and their severity. Be open about both physical and emotional symptoms; they are all pieces of the puzzle.
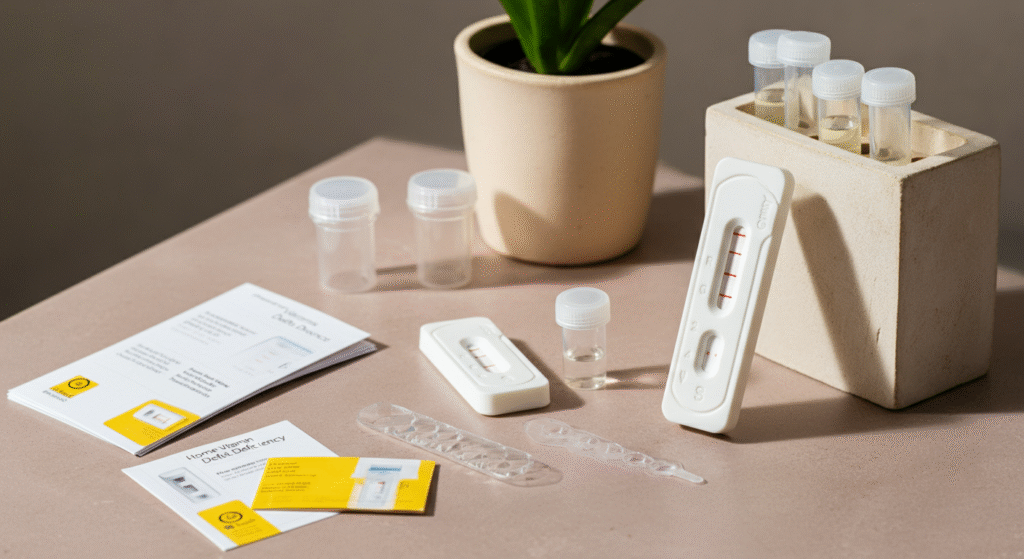
Hormone Testing
To get a clear picture of what is happening inside your body, your doctor will likely order specific tests.
Blood Tests
Bloodwork is the most common diagnostic tool. Your provider may check:
- hCG: To confirm that pregnancy hormone levels have returned to zero.
- Thyroid Panel (TSH, T3, T4): To rule out postpartum thyroiditis or general thyroid dysfunction.
- Progesterone and Estrogen: To see if these sex hormones are rebalancing correctly in relation to your cycle.
- FSH and LH: To evaluate ovarian function.
Saliva or Urine Tests
While less standard in conventional settings, some functional medicine practitioners may use saliva or dried urine testing (like the DUTCH test) to look at how your body metabolizes hormones throughout the day, providing a more nuanced look at cortisol and hormone byproducts.
Paths to Rebalancing Your Hormones
Once you understand what is happening, you can take proactive steps to support your body. Healing is rarely about a single “fix” but rather a combination of lifestyle changes and, when necessary, medical intervention.
Lifestyle and Natural Support
Nutrition for Recovery
Food is information for your hormones. Focus on a nutrient-dense diet rich in whole foods. Healthy fats (like avocados, olive oil, and nuts) are essential building blocks for hormone production. High-quality proteins help repair tissue and stabilize blood sugar, which keeps cortisol in check.
Consider adding foods rich in:
- Omega-3 fatty acids: Found in fatty fish and flaxseeds, these reduce inflammation.
- B Vitamins: Found in leafy greens and legumes, these support energy and mood regulation.
- Iron: Essential if you experienced heavy bleeding.
Gentle Movement
While you might not feel ready for high-intensity workouts, movement is vital for processing stress hormones. Engage in gentle exercises like walking, restorative yoga, or stretching. These activities help regulate insulin and cortisol without placing additional stress on a recovering body.
Stress Management
Because cortisol steals resources from other hormones (like progesterone), managing stress is non-negotiable. Techniques such as mindfulness meditation, deep breathing exercises, or journaling can help lower your stress baseline. Allowing yourself space to grieve without judgment is also a form of stress management.
Medical Treatments
Hormone Therapy
If testing reveals significant deficiencies, your doctor might suggest bioidentical hormone replacement therapy (BHRT). For example, progesterone supplements taken during the second half of your cycle can help regulate periods and improve sleep.
Medication for Specific Symptoms
In some cases, the hormonal drop triggers severe mental health struggles. Antidepressants or anti-anxiety medications can serve as a bridge, helping you manage symptoms while your body finds its equilibrium. This does not mean you will be on medication forever; it is a tool to help you cope during a crisis.
Thyroid Medication
If blood tests reveal that your thyroid is underactive or overactive, specific medications (like levothyroxine) may be prescribed to restore proper function. Thyroid health is critical for overall energy and metabolism.
FAQs About Post-Miscarriage Hormones
How long do pregnancy hormones stay in your body after a miscarriage?
It varies depending on how far along the pregnancy was. Generally, hCG levels return to zero within 2 to 4 weeks, but for some, it can take up to 6 weeks. Other hormones like estrogen and progesterone usually drop more sharply immediately following the loss.
Can a miscarriage cause permanent hormone imbalance?
Typically, hormone imbalances after a miscarriage are temporary. The body is resilient and usually strives to return to homeostasis. However, for some women, the stress of the event can trigger underlying issues like thyroid dysfunction or adrenal fatigue that may require longer-term management.
Should I see an endocrinologist or my OB-GYN?
Start with your OB-GYN, as they are most familiar with your reproductive history. However, if symptoms persist or complex issues like thyroid disease arise, a referral to a reproductive endocrinologist may be beneficial.
Supporting Your Recovery Journey
Recognizing the signs of hormone imbalance after a miscarriage is an act of self-compassion. It affirms that what you are experiencing is real and that it is a medical issue deserving of care, not just something you have to “get over.”
Healing is a nonlinear journey. It involves repairing the physical body while tending to a broken heart. Be patient with yourself. If you recognize these symptoms, reach out to a healthcare provider who listens to you.
You do not have to navigate this alone. Whether it is through medical intervention, nutritional support, or counseling, resources are available to help you feel like yourself again.